The Sciatic Nerve: Its Pathway, Compression Points, and Holistic Approaches to Relief
The sciatic nerve is the longest and thickest nerve in your body, playing a vital role in lower limb function and mobility. Originating from the lumbar and sacral plexus, it travels down the spine, through the pelvis, and into the legs, branching off to deliver motor and sensory signals. But due to its long journey, it's prone to compression and irritation, which can cause pain, numbness, and dysfunction. In this post, we’ll explore its pathway, common compression points, how hysterectomies and sacral damage can impact it, and most importantly, how you can take charge of your recovery with Hypopressives, breathwork, foot mechanics, and release techniques.
The Sciatic Nerve’s Journey: From Origin to Insertion
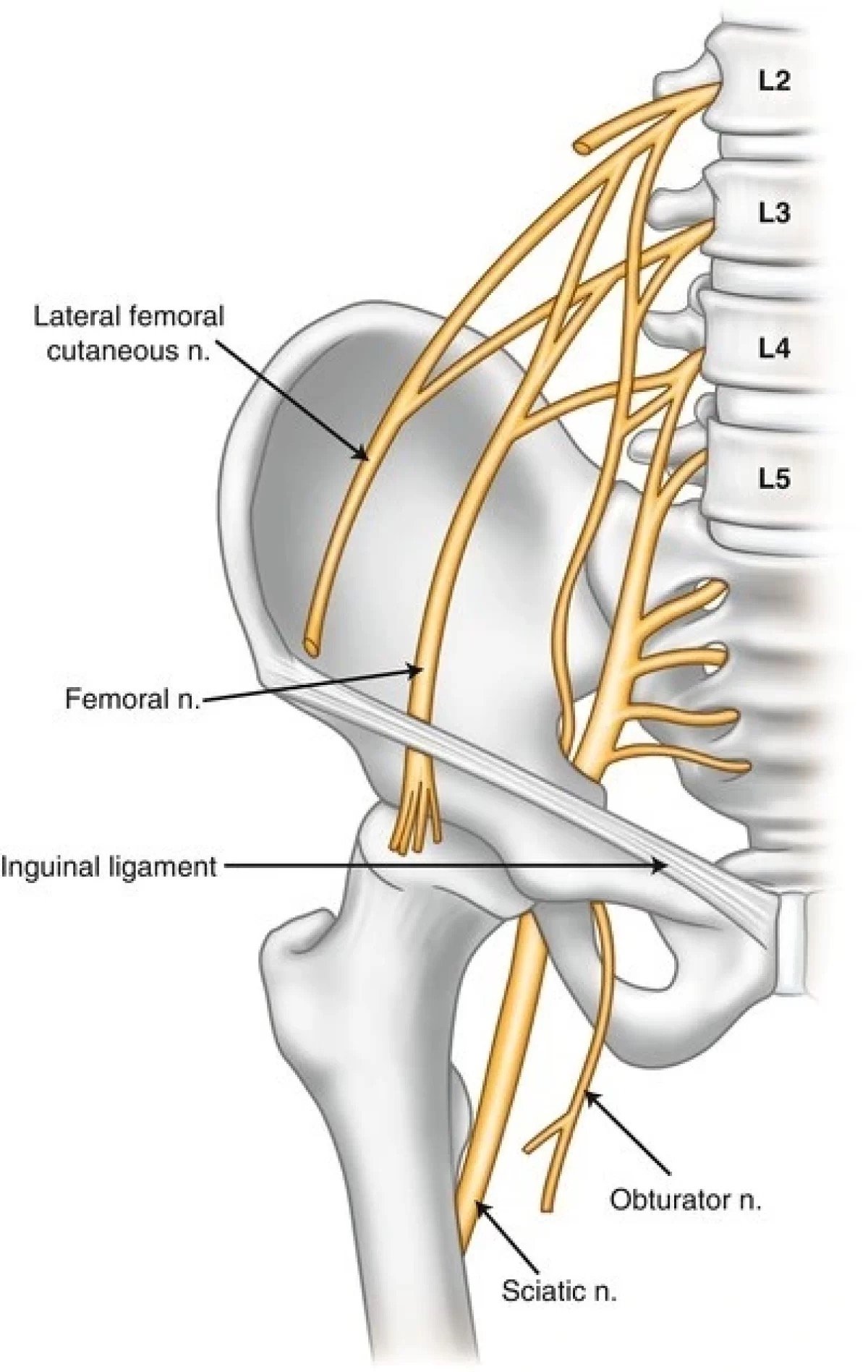
The sciatic nerve originates from the L4-S3 nerve roots of the lumbosacral plexus, exiting the spinal column through the greater sciatic notch of the pelvis. From there, it travels down the gluteal region, running beneath (or sometimes through) the piriformis muscle, and continues along the posterior thigh. Near the knee, it divides into two main branches:
The tibial nerve, which controls the muscles and sensation of the posterior lower leg and foot.
The common peroneal (fibular) nerve, which wraps around the fibular head and supplies the front and outer lower leg and foot.
With such a vast reach, any compression along its path can impact mobility and cause discomfort.
Key Points of Compression
The sciatic nerve can get trapped or irritated at several points, including:
The Lumbar Spine (L4-S1) – Issues like disc herniation, degeneration, or poor spinal alignment can put pressure on the nerve roots.
The Piriformis Muscle – If the nerve passes through rather than beneath this muscle, tightness or spasms can cause compression (Piriformis Syndrome).
The Sacroiliac Joint and Sacral Region – Misalignment or dysfunction here can contribute to sciatic irritation.
The Ischial Tuberosity (Sitting Bones) – Prolonged sitting can put direct pressure on the nerve.
The Fibular Head – Compression here can lead to issues such as foot drop and gait abnormalities.
Effects of Hysterectomies and Sacral Damage on the Sciatic Nerve
Pelvic surgeries, especially hysterectomies, can have lasting effects on the sciatic nerve:
Scar tissue formation can create adhesions around the nerve, limiting movement and increasing irritation.
Changes in intra-abdominal pressure can shift pelvic alignment, leading to secondary compression.
Pelvic floor dysfunction post-surgery may alter posture and contribute to nerve entrapment.
Sacral damage or instability, whether from surgery, trauma, or long-term stress, can disrupt the nerve’s pathway and cause chronic irritation.
Self-Help Strategies for Sciatic Nerve Health
The McKenzie Method: A Targeted Approach to Sciatica Relief
Developed by physiotherapist Robin McKenzie in the 1950s, the McKenzie Method is a globally recognised system for assessing and treating spinal conditions, including sciatica. It focuses on identifying specific movement patterns that relieve nerve compression and promote spinal health. The goal is to empower individuals to take an active role in their recovery by using targeted exercises to centralise pain and improve mobility.
The McKenzie Method is a simple yet effective way to manage sciatic pain and improve spinal function. This self-guided approach focuses on realigning the spine and reducing nerve irritation through specific movements.
The 7 Key McKenzie Exercises are designed to progressively restore function and alleviate nerve irritation. These movements help reposition intervertebral discs, reduce inflammation, and improve spinal extension, which can be particularly beneficial for sciatica. Here’s how each exercise works:
Prone Lying – This is the starting position for many McKenzie exercises. Simply lying on your stomach allows the lumbar spine to settle into a neutral position, relieving initial pressure on the sciatic nerve.
Prone on Elbows – By propping up on your elbows, you encourage a gentle extension in the lower back, which can help move bulging discs away from the nerve root and reduce sciatic pain.
Press-Ups (Prone Extension) – A more advanced extension exercise, press-ups further open up the lumbar spine, helping to centralise pain and restore normal nerve function.
Standing Extension – Performed by placing hands on the lower back and gently arching backwards, this exercise reinforces spinal extension and encourages disc realignment in a functional standing position.
Flexion in Lying – This movement gently stretches the lower back and posterior chain, helping to relieve tension in tight lumbar muscles and improve nerve glide.
Flexion in Sitting – This seated variation of forward flexion can provide relief by creating space in the lower back, especially for those with stiffness or postural imbalances.
Flexion in Standing – A functional way to enhance mobility, this movement encourages lumbar flexibility and facilitates proper nerve glide along the lower limb.
These movements encourage better spinal function and help free up the sciatic nerve, making daily movement smoother and more comfortable.
Additional Holistic Strategies for Sciatic Relief
1. Hypopressives and Breathwork
Hypopressives help reduce intra-abdominal pressure and decompress the spine, which can relieve sciatic tension.
Diaphragmatic breathing stimulates the parasympathetic nervous system, calming the body and reducing muscular tension around the nerve.
Breath-coordinated movement enhances postural alignment, ensuring better nerve glide and less compression.
2. Footwork and Biomechanics
The sciatic nerve runs all the way to the feet, so dysfunctional foot mechanics can create tension further up the chain.
Strengthening the intrinsic foot muscles, improving ankle mobility, and ensuring even weight distribution can reduce nerve stress.
Rolling the soles of the feet on a soft ball helps stimulate neural pathways and improve nerve mobility.
3. Release Techniques for Sciatic Nerve Relief
Piriformis and Glute Release – Gentle myofascial work in the glutes can ease sciatic compression.
Lumbar and Sacral Mobilisation – Subtle spinal movements and sacral releases promote fluidity and nerve function.
Nerve Glide Exercises – Specific neural mobilisation techniques allow the sciatic nerve to move freely along its pathway.
Bringing It All Together
The sciatic nerve plays a crucial role in movement, and when it’s irritated, it can seriously disrupt daily life. Whether the cause is postural misalignment, surgical intervention, or sacral dysfunction, addressing sciatic nerve health requires a whole-body approach.
By integrating Hypopressives, breathwork, foot mechanics, and targeted release techniques, you can create space for your sciatic nerve to glide freely, reduce tension, and restore balance to your body.
If sciatica is holding you back, don’t just push through it—take an active role in your recovery. Explore these holistic strategies, reconnect with your movement, and regain comfort. And if symptoms persist, a healthcare professional can offer tailored guidance to support your journey back to pain-free movement.