Insights
Pathways to Pain Relief: Insights and Resources for Your Journey
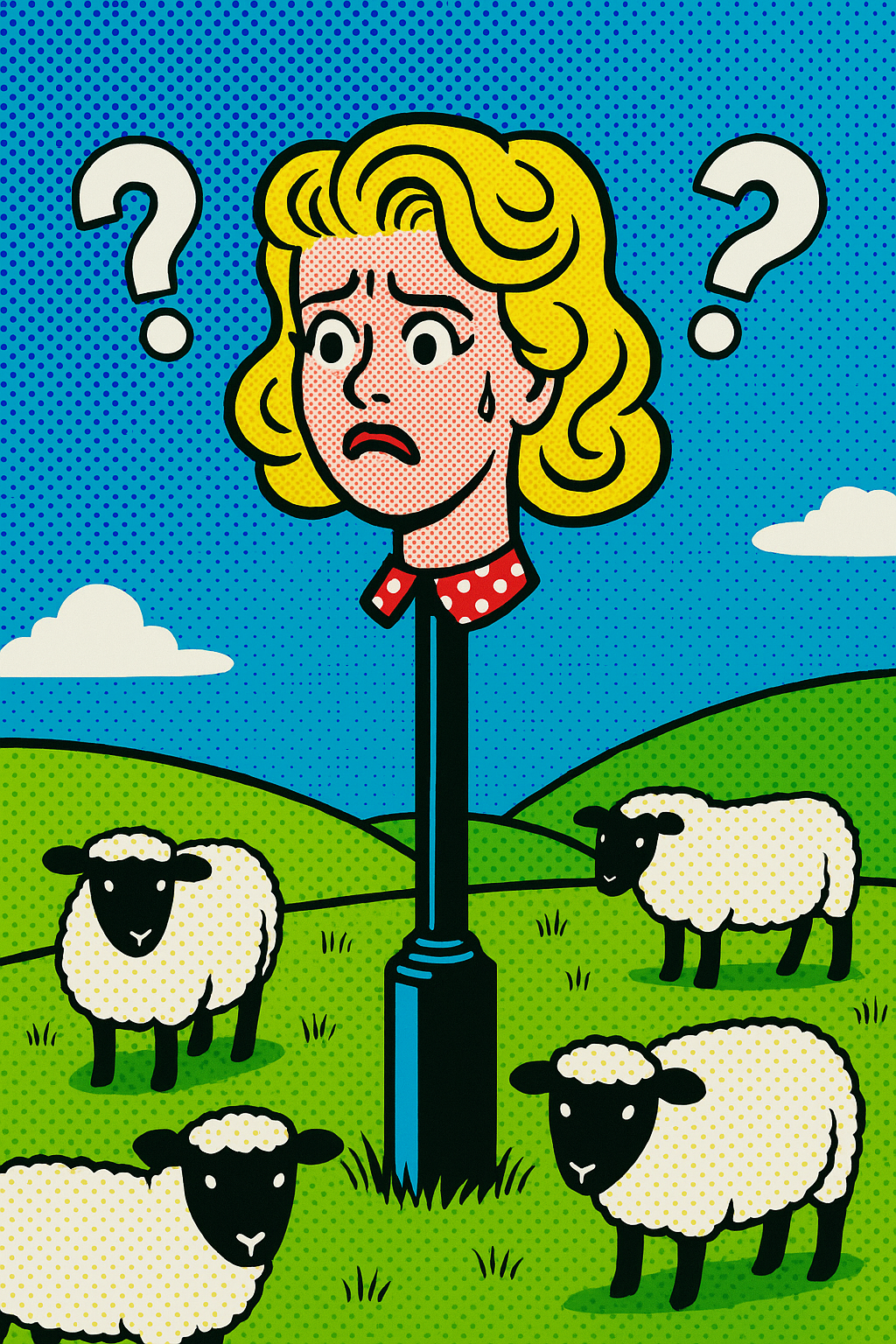
The Mind–Pelvis Connection: How Emotions, Trauma and Stress Affect Pelvic Floor Health
Many people experience pelvic floor symptoms without any clear injury, diagnosis or structural explanation. These can appear as tightness, pain, leaking, heaviness or even a feeling of gripping or just feeling disconnected.
Scans and tests often come back “normal”, yet the symptoms persist. This can be deeply frustrating and confusing, especially when you believe you are doing all the “right” things.
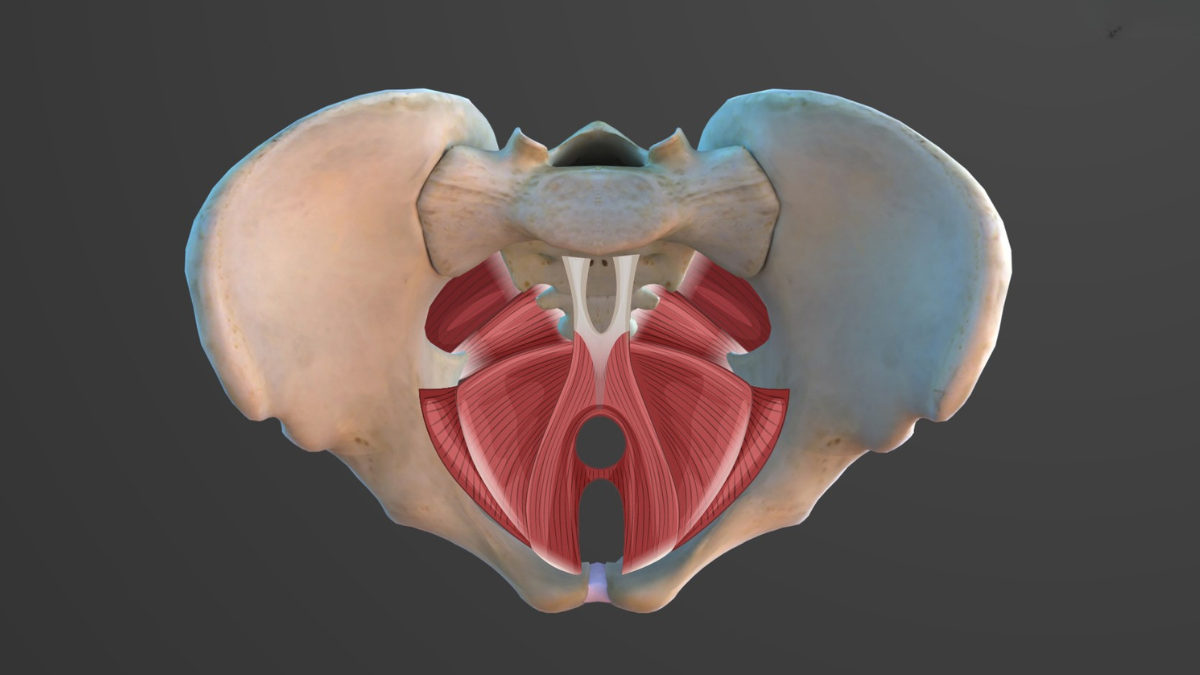
Increasingly, research and clinical experience are highlighting the mind–body pelvic floor connection. The pelvis is not just a set of muscles. It is part of a complex system shaped by emotions, stress, trauma, breath and the nervous system.
Can Hypopressives Help with Prolapse? Natural Support for Bladder, Uterus & Bowel Health
If you are living with prolapse symptoms, you are not weak, failing, or broken. You are one of many women navigating changes in the body that are far more common than most of us were ever told.
Bladder, uterine and bowel prolapse affect a significant number of women, particularly after pregnancy and birth, and again during peri-menopause and menopause. Many describe a feeling of heaviness, dragging, pressure or a bulge. Others notice leaking, discomfort with exercise, or a sense that their body no longer feels supportive or reliable.
The Femoral Cutaneous Nerve: The Overlooked Nerve That Can Mimic Pelvic, Hip & Thigh Pain
Femoral cutaneous nerve irritation doesn’t feel like a pulled muscle.
Women often describe: Burning or heat across the thigh, tingling or pins and needles, numb patches, a buzzing or electric quality, pain that worsens with standing, walking or tight clothing
And crucially: It may ease when sitting or lying, stretching the thigh often doesn’t help, strength work can make it worse
Pelvic Floor Restoration vs Pelvic Floor Management: What’s the Difference?
Why pelvic floor restoration is different
Pelvic floor restoration is not about doing more.
It’s about changing the relationship you have with your body.
Restoration focuses on:
helping the body feel safe again
reducing nervous system vigilance
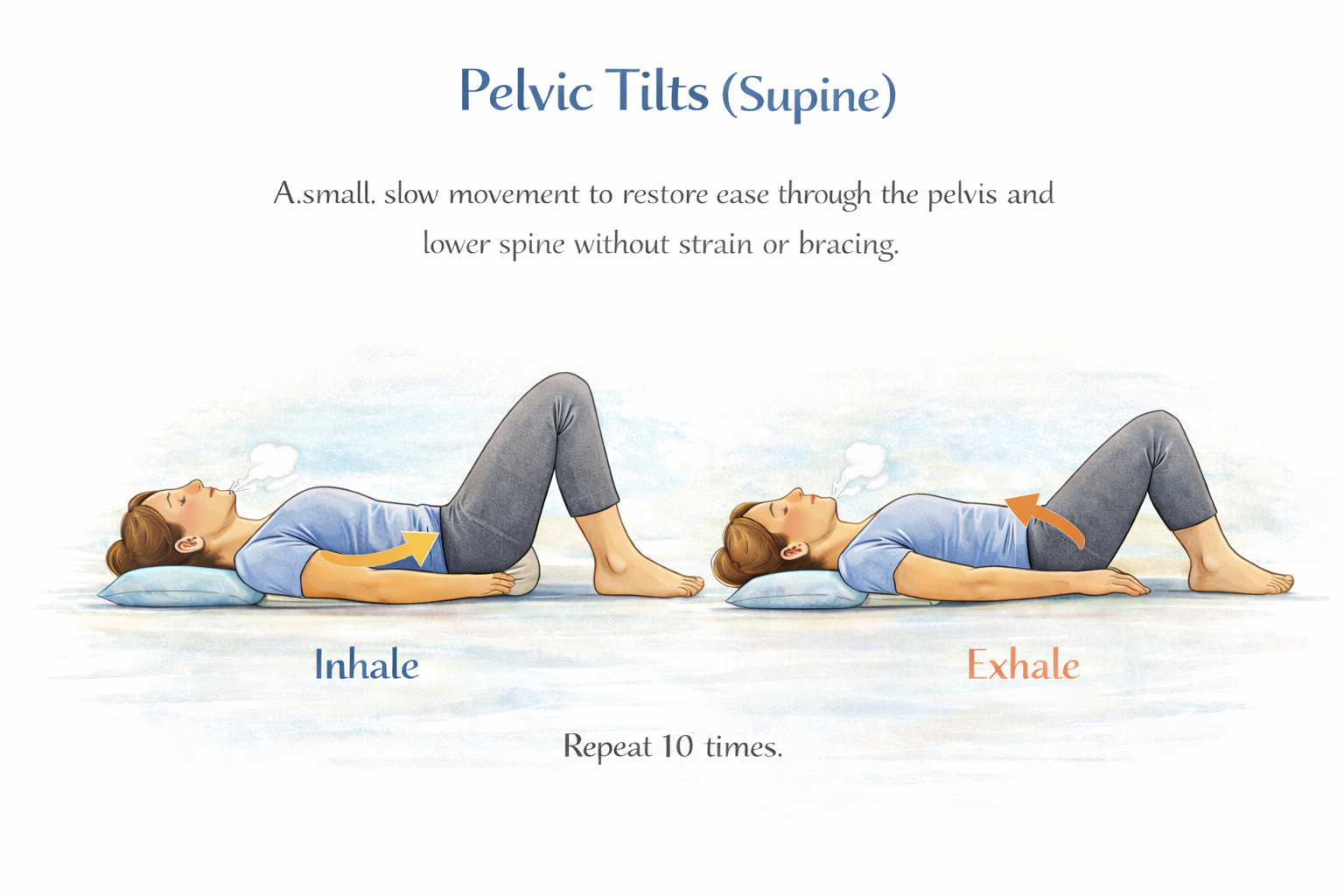
restoring natural coordination between breath, pressure, and support
rebuilding confidence through gradual, real-life movement
Rather than asking you to control your body, restoration helps your body relearn how to support you.
The goal isn’t perfection.
The goal is trust.
Training with Hypermobility & hEDS: Why “Being Flexible” Isn’t the Problem
What’s really going on in a hypermobile body?
With hEDS, the connective tissue that usually provides passive joint support is more elastic. That means the body has to rely much more on:
Muscle timing
Nervous system responses
Proprioception (your sense of where you are in space)
So instead of feeling solid and predictable, the body can feel:
Floaty or unstable
Over-alert
Or paradoxically… very tight
That tightness isn’t strength — it’s protection.
Many hypermobile people are both bendy and braced at the same time.
5 Things You Can Do Today to Help Your Pelvic Floor
Most women I work with haven’t done “nothing”.
They’ve done too much, in the wrong order.
So here are five things you can do today that actually support your pelvic floor — not by forcing it to behave, but by giving it the conditions it needs to respond.
Pelvic Floor Myths vs Reality: Why “Just Do Your Kegels” Often Isn’t the Answer
If I Make My Pelvic Floor Tighter, I’ll Be Stronger
This is one of the most common misunderstandings — and one of the most damaging.
Tightness feels like control.
It feels like effort.
It feels like you’re doing something.
But tight isn’t the same as strong.
A muscle that’s always gripping is often tired, under-oxygenated, and struggling to respond when it actually needs to. Many people with pelvic floor symptoms are already holding — through their belly, jaw, shoulders, glutes, breath — without even realising it.
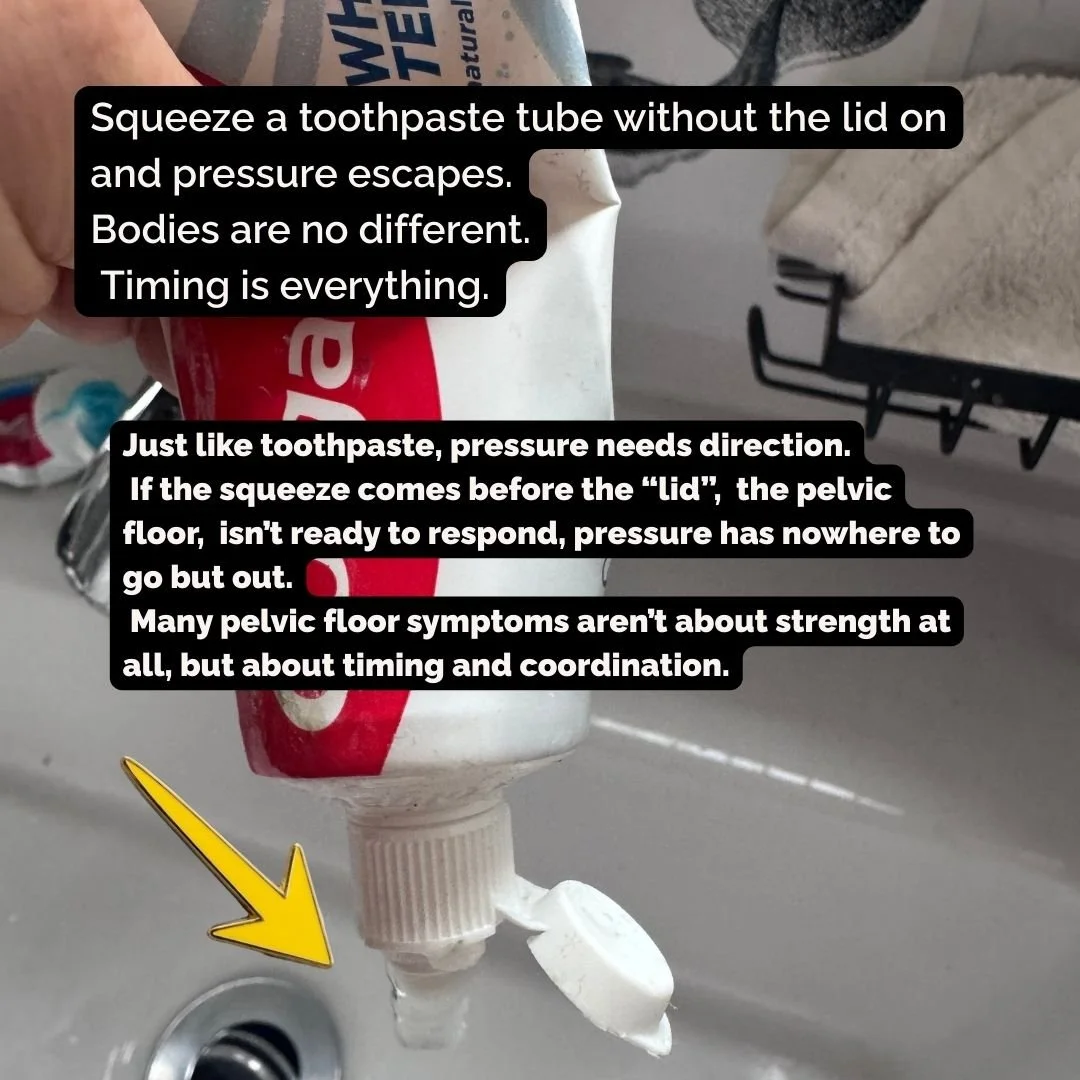
Breath Holds, Vacuums & the Pelvic Floor
Healing and training the pelvic floor is not about choosing one method.
It’s about sequence.
Just as a personal trainer wouldn’t load strength onto a stiff, guarded body, we don’t ask the pelvic floor to “work harder” before it knows how to release, move, coordinate and recover.
TRE® helps reduce chronic tension and trauma-driven guarding, restoring a baseline sense of safety in the nervous system.
Hypopressives then restore posture, breath timing, pressure management and fascial expandability — allowing an internal lift through passive recoil, organ repositioning and reflexive pelvic floor response. This is mobility and coordination training for the pelvic floor, supported by intermittent hypoxia and cellular adaptation.
Only then do we layer in Pelvic Floor Muscle Training (PFMT) — the strength work that builds urethral and vaginal closure, resting tone and endurance.
Just as strength training without mobility creates stiff, non-functional “gym strong” bodies, pelvic floor strength without mobility and coordination fails to solve pressure problems.
The Vagus Nerve, the Heart, the Diaphragm
You may have heard the vagus nerve described as the calming nerve , or been told to “stimulate it” with breathing exercises, humming, or slow exhales.
That idea isn’t wrong.
But it’s incomplete.
The vagus nerve isn’t a switch you turn on. It’s part of a communication network linking your brain, heart, breath, diaphragm, gut , and indirectly, your pelvic floor.
Understanding this network helps explain why breath, posture, pressure, and nervous-system awareness matter so much in pelvic health.
Some Most Embarrassing Things That Happen With Pelvic Floor Dysfunction
Let’s have a slightly uncomfortable but very necessary chat.
Because if you’ve ever:
• crossed your legs before sneezing
• planned walks based on toilet locations
• avoided jumping, laughing or yoga “just in case”
• worn your safe pants (you know the ones)
…welcome. You’re in extremely good company.
Here’s the thing no one tells you:
Most “embarrassing” pelvic floor stuff isn’t because your body is weak.
It’s because it’s working overtime trying to protect you.
The clitoris. Where it actually is, how it moves, and why your nervous system cares
This part fascinates me.
The clitoris isn’t static.
It responds to breath, pressure changes, arousal, and relaxation.
When the nervous system feels safe:
Blood flow increases
The tissues gently engorge and lift
The bulbs and crura subtly expand and recoil
Sensation feels warm, alive, connected
When the system feels threatened or overloaded:
The tissues may stay guarded
Sensation can feel dulled, buzzy, or overwhelming
Movement becomes restricted — not because anything is “wrong,” but because the body is protecting
This is why pelvic floor tension and clitoral sensation are so closely linked.
A gripping pelvic floor doesn’t just affect continence or prolapse , it changes how pleasure is perceived.
How Smiling Supports Your Nervous System (and Why That Matters for Pelvic Floor Health)
Smiling won’t fix your pelvic floor.
But it can change the conditions your pelvic floor is working under, and that can make a real difference.
Your Spine: The Highway of Movement, Breath & Pelvic Floor Health
Why your spine isn’t just a stack of bones, it’s your body’s communication superhighway
Grief Lives in the Lungs: When Breath Holds What the Heart Can’t
There are some emotions the mind can’t process right away
so the body steps in and protects us.
And the lungs — the place where life arrives breath by breath —
are often where grief takes shelter first.
If you’ve ever felt heartbreak as tightness in your chest, or loss as a collapse in your ribcage, you’ve already felt this truth:
Your breath holds what your heart can’t handle yet.