Pelvic Floor Muscles, Organs, and the Impact of Scar Tissue in Female Pelvic Health
Understanding the Pelvic Floor: A Foundation of Support
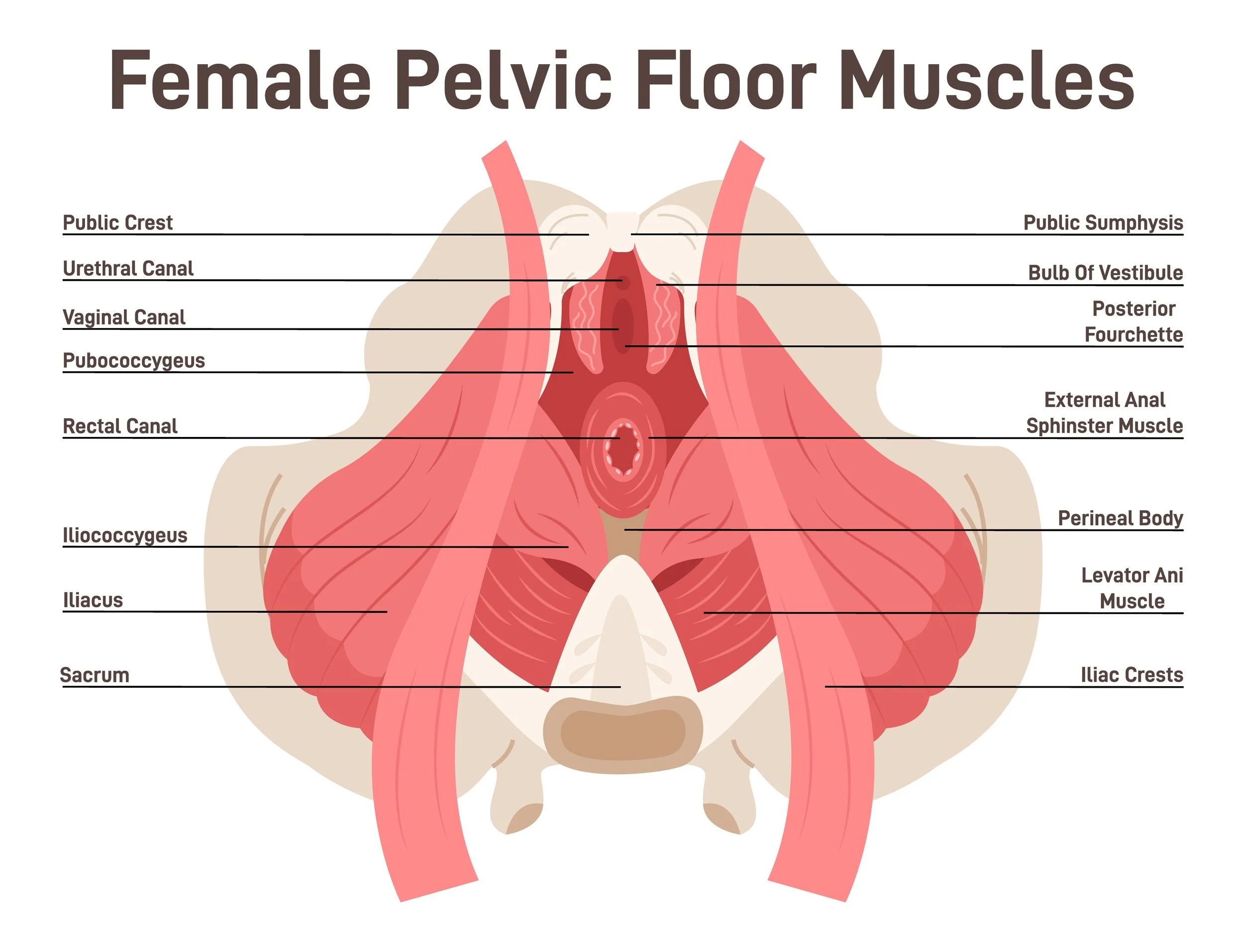
The pelvic floor is a complex web of muscles, fascia, and connective tissue that provides essential support for the bladder, uterus, and rectum. These muscles work in harmony to maintain continence, stabilise posture, facilitate childbirth, and contribute to sexual function.
The pelvic floor is made up of several layers, with key muscles including:
Levator Ani Group (Pubococcygeus, Puborectalis, Iliococcygeus) – The primary support system for pelvic organs.
Coccygeus Muscle – Aids in stabilising the sacrum and tailbone.
Perineal Muscles – Including the deep and superficial transverse perineal muscles, bulbospongiosus, and ischiocavernosus, which support vaginal and urethral function.
When functioning optimally, the pelvic floor maintains organ position, controls pressure distribution within the core, and prevents prolapse and incontinence. However, when scar tissue forms within this region, complications can arise that significantly impact quality of life.
Pelvic Organs and How They Are Affected by Scar Tissue
The female pelvic floor cradles three primary organs:
Bladder & Urethra – Controlling urinary continence and voiding.
Uterus & Vagina – Playing key roles in reproductive and sexual health.
Rectum & Anus – Managing bowel movements and continence.
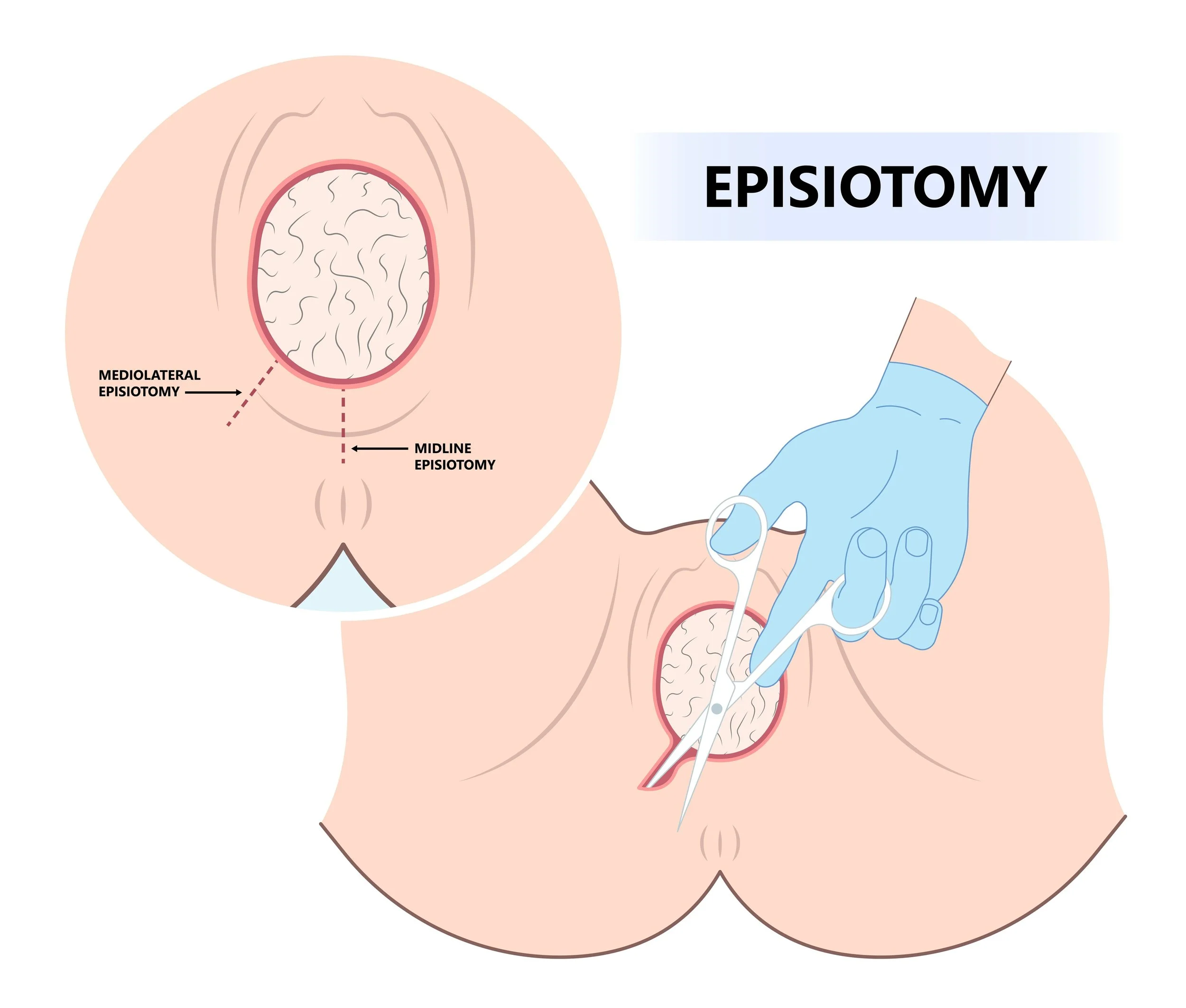
Scar tissue—whether from childbirth, surgery (such as a C-section, hysterectomy, or episiotomy), endometriosis, or pelvic infections—can create adhesions that tether these organs together. This can result in:
Bladder dysfunction: Urgency, frequency, or difficulty voiding.
Painful intercourse (dyspareunia): Due to restricted tissue mobility.
Bowel dysfunction: Including constipation or pain with defecation.
Pelvic organ prolapse: Due to imbalanced fascial support.
The Silent Grip of Scar Tissue on the Pelvic Floor
Scar tissue forms as part of the body's healing process following injury, surgery, or inflammation. Unlike normal, pliable fascia, unmobilised scar tissue is dense, fibrotic, and less elastic, often binding tissues together in ways that restrict natural movement. This leads to:
Reduced nerve glide: Resulting in numbness, tingling, or referred pain in the pelvis, lower back, and legs.
Fascial dehydration: Scarred fascia lacks the same hydration and mobility as healthy connective tissue, exacerbating stiffness and discomfort.
Tugging forces across muscle chains: Scar adhesions can create a ripple effect, pulling through the biotensegrity of the entire body, affecting posture and causing compensatory movement patterns.
Insights from Gil Hedley and Diane Lee on Scar Tissue and Adhesions
Renowned anatomist Gil Hedley has extensively studied the impact of scar tissue on fascia and body-wide movement. He describes how adhesions act like "fascial Velcro," limiting mobility and altering natural movement patterns. His work highlights the importance of hydration, movement, and manual release in restoring fascial glide, particularly in the pelvis, where adhesions can disrupt the synergy between the pelvic floor, diaphragm, and core. Hedley emphasises that movement is key in breaking down restrictive adhesions, as fascia responds dynamically to load, stretch, and pressure changes.
Meanwhile, Diane Lee, a leading expert in physiotherapy and integrative movement, emphasises the role of intra-abdominal pressure regulation in pelvic health. She explains how scar adhesions can disrupt the core canister—the functional relationship between the diaphragm, abdominal wall, and pelvic floor. When these structures are restricted, compensations arise, increasing the likelihood of pelvic organ prolapse and chronic pain. Diane Lee advocates for dynamic core integration through breathwork, postural alignment, and manual therapy to re-establish functional stability. Her clinical research also supports a holistic approach, combining fascial release with neuromuscular retraining to restore optimal core function.
Anna Crowle’s Work on Scar Tissue Adhesions and Prolapse
Anna Crowle’s research and clinical work on scar tissue adhesions highlight how fascial restrictions can contribute to pelvic organ prolapse. Her findings suggest that scar tissue from surgical interventions, such as C-sections or perineal repairs, can create tension across the pelvic fascia, altering the natural mobility of the pelvic organs. These adhesions can:
Disrupt intra-abdominal pressure balance, causing organs to shift downward.
Prevent optimal pelvic floor engagement, leading to weakness and prolapse progression.
Cause referred pain and dysfunction by altering nerve pathways within the pelvic region.
Crowle’s approach to treatment focuses on restoring fascial glide and elasticity through hands-on techniques like visceral manipulation, myofascial release, and functional movement. She also highlights the need for scar-specific mobilisation exercises, which help reintroduce elasticity into the tissue, reducing restrictions and promoting fluidity in movement. Additionally, she emphasises the importance of neuromuscular coordination, ensuring that the pelvic floor muscles regain their natural ability to contract and release without being restricted by adhesions.
How and Why Hypopressives Help with Scar Tissue and Prolapse
Hypopressives are a powerful tool for addressing scar tissue restrictions and preventing or managing pelvic organ prolapse. Unlike traditional core exercises, which often increase intra-abdominal pressure, Hypopressives work by reducing downward pressure while enhancing the lift and support of the pelvic floor. Here’s how:
Myofascial Release & Tissue Hydration: The vacuum effect created during the Hypopressive breath helps mobilise fascial layers, increasing blood flow and reducing adhesions.
Improved Pressure Regulation: The apnoea phase (breath-hold with rib expansion) decompresses the pelvic cavity, lifting organs and counteracting the effects of gravity on prolapse.
Neurodynamic Stimulation: By engaging deep core muscles, Hypopressives activate the nervous system, improving coordination between the diaphragm, pelvic floor, and core.
Reintegration of Movement Patterns: Hypopressive postures promote optimal alignment and pelvic stability, ensuring that movement does not exacerbate pressure-related dysfunction.
Addressing Scar Tissue for Pelvic Floor Health
Thankfully, there are holistic strategies to improve mobility, reduce discomfort, and restore function within the pelvic floor:
Myofascial Release & Scar Tissue Mobilisation
Manual therapy, such as visceral manipulation or internal pelvic floor release, can help soften adhesions and improve tissue glide.
Hypopressives & Breathwork
Hypopressive exercises encourage decompression of the pelvic region, reducing excessive intra-abdominal pressure and promoting myofascial mobility.
360° Lateral Costal Breathing hydrates and mobilises fascia, improving circulation to scarred areas.
Neurodynamic Mobilisation
Gentle nerve gliding techniques help free restrictions within the nervous system, easing symptoms like pelvic pain or tingling.
Postural Awareness & Movement Therapy
Realigning posture and retraining movement patterns can prevent compensatory dysfunction caused by restricted tissue.
Hydration & Nutrient Support
Supporting fascial health with adequate water intake, collagen-rich foods, and anti-inflammatory nutrients can enhance tissue repair.
Final Thoughts: Healing is Possible
Scar tissue may alter the landscape of the pelvic floor, but it doesn’t have to define its function. By addressing these restrictions with a combination of hands-on techniques, breathwork, and postural awareness, women can regain strength, comfort, and confidence in their bodies.
If you’re struggling with pelvic floor dysfunction, you don’t have to navigate this alone. There is support available, and healing is absolutely possible.