Insights
Pathways to Pain Relief: Insights and Resources for Your Journey
Slow Down: The Truth About Apnoea Practice and Pelvic Floor Health
There’s something that’s been bothering me lately, and I need to get it off my chest. Some clients are being told by PT trainers and physios that the goal is to do 30 apnoeas per session—as if hitting that magic number is the secret to pelvic floor perfection. It’s almost as if these practitioners just can’t quite let go of their Kegel fixation—count, squeeze, repeat.
But here’s the thing: That’s not how Hypopressives—or your pelvic floor—actually work.
Why Kegels May Not Be the Best Choice for Most Women with Pelvic Floor Dysfunction
Your pelvic floor isn’t meant to work in isolation—it’s part of a complex, coordinated team. It works alongside your diaphragm, deep core, hips, feet, and nervous system.
What your body really needs is a responsive pelvic floor:
One that contracts when needed, relaxes when it’s safe, and moves rhythmically with your breath and posture.
Kegels isolate the pelvic floor from this team. They often fail to restore true function—and can even create further imbalance.
How Hypopressives and Apnoeas Impact the Fascia, Pelvic Organs, and Pelvic Floor
In Hypopressives, we’re always focusing on creating an elongated, neutral spine and stacking the ribcage efficiently over the pelvis. This alignment supports the vacuum effect, allowing the fascia to move upward in a more balanced, unrestricted way. It also means that the pelvic floor reflexively responds to this pressure shift without any conscious squeezing or bracing. The abdominal muscles, particularly the deeper ones like the transversus abdominis, cinch inward naturally, creating a corset-like effect without forcing a contraction.
The Role of Nerve Flossing, Arm Spirals, and Gentle Lengthening in Hypopressives
Nerve flossing with arm spirals and active gentle lengthening in Hypopressives is a powerful yet often overlooked tool for improving nerve glide, fascial hydration, and neuromuscular efficiency. When executed correctly, these movements not only mobilise restricted nerves but also help integrate the entire body’s postural, respiratory, and neurological systems for improved function and pelvic floor health.
Pelvic Floor Muscles, Organs, and the Impact of Scar Tissue in Female Pelvic Health
The pelvic floor is a complex web of muscles, fascia, and connective tissue that provides essential support for the bladder, uterus, and rectum. These muscles work in harmony to maintain continence, stabilise posture, facilitate childbirth, and contribute to sexual function.
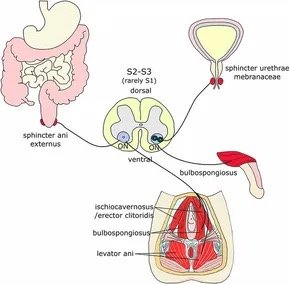
The pelvic floor is made up of several layers, with key muscles including:
Levator Ani Group (Pubococcygeus, Puborectalis, Iliococcygeus) – The primary support system for pelvic organs.
Coccygeus Muscle – Aids in stabilising the sacrum and tailbone.
Perineal Muscles – Including the deep and superficial transverse perineal muscles, bulbospongiosus, and ischiocavernosus, which support vaginal and urethral function.
When functioning optimally, the pelvic floor maintains organ position, controls pressure distribution within the core, and prevents prolapse and incontinence. However, when scar tissue forms within this region, complications can arise that significantly impact quality of life.
The Nervous System, Bladder Control, and Incontinence: A Deep Dive into Polyvagal Theory, the Onuf’s Nucleus, and Bladder Training
Bladder dysfunction is not just a mechanical issue—it’s deeply connected to the nervous system. By understanding the role of Polyvagal Theory, Onuf’s nucleus, and bladder retraining, we can take a multifaceted approach to restoring urinary function.
💡 Key Takeaways: ✔ The autonomic nervous system plays a crucial role in bladder control.
✔ Stress and trauma can disrupt the bladder’s normal function.
✔ Bladder retraining and nervous system regulation improve continence.
✔ Hypopressives are a powerful tool to regulate intra-abdominal pressure and support bladder health.
✔ Balanced pelvic floor muscle tone is key—neither too tight nor too weak—for optimal continence.
For those struggling with bladder dysfunction or incontinence, a combined approach of bladder training, breathwork, pelvic floor support, and nervous system regulation offers real solutions for long-term relief.
✨ Let’s start normalising conversations around bladder health and give our nervous systems the care they need! ✨
Onuf’s Nucleus: The Tiny Powerhouse That Controls Your Pelvic Floor (And Why Hypopressives Can Help!)
Onuf’s nucleus. You may not have heard of it, but it’s working hard for you every day—helping you control your bladder and bowels, keeping your pelvic floor muscles engaged, and even playing a role in orgasmic contractions(yes it also helps with amazing orgasims)
Scar Tissue, Fascia, and the Ripple Effect on the Pelvic Floor: How Breath and Posture Can Help
Scar tissue is a natural part of the body’s healing process after a hysterectomy, pelvic floor surgery, or any abdominal intervention. However, while it serves as the body's internal "patchwork," it doesn’t always integrate seamlessly into the surrounding tissues. Instead, scar tissue can form adhesions—dense, fibrous bands that create restrictions and pull through the biotensegrity of the entire body.
This post will explore how these adhesions impact movement, hydration, and nerve glide within the fascia and muscle chains—and how postural awareness and Hypopressives can be powerful tools in restoring balance and function.
The Emotional Blueprint of the Pelvic Floor: How Thoughts, Movement, and the Nervous System Shape Function
Dorsal Vagal (Freeze/Fawn):
Unlike fight-or-flight, where the pelvic floor tightens in response to stress, freeze mode causes a sense of disconnection from the body.
Women often cannot fight or flee from their own pelvic floors, so they may instead freeze, resulting in a lack of sensation, dissociation, or numbness in the pelvic area.
The fascia becomes rigid and dry, reducing mobility and increasing pain perception.
Bladder function may be affected by delayed or absent signals, leading to retention or leaks due to an unresponsive pelvic floor.
Movement feels slow, heavy, or disconnected, and engaging with the pelvic area may feel overwhelming.
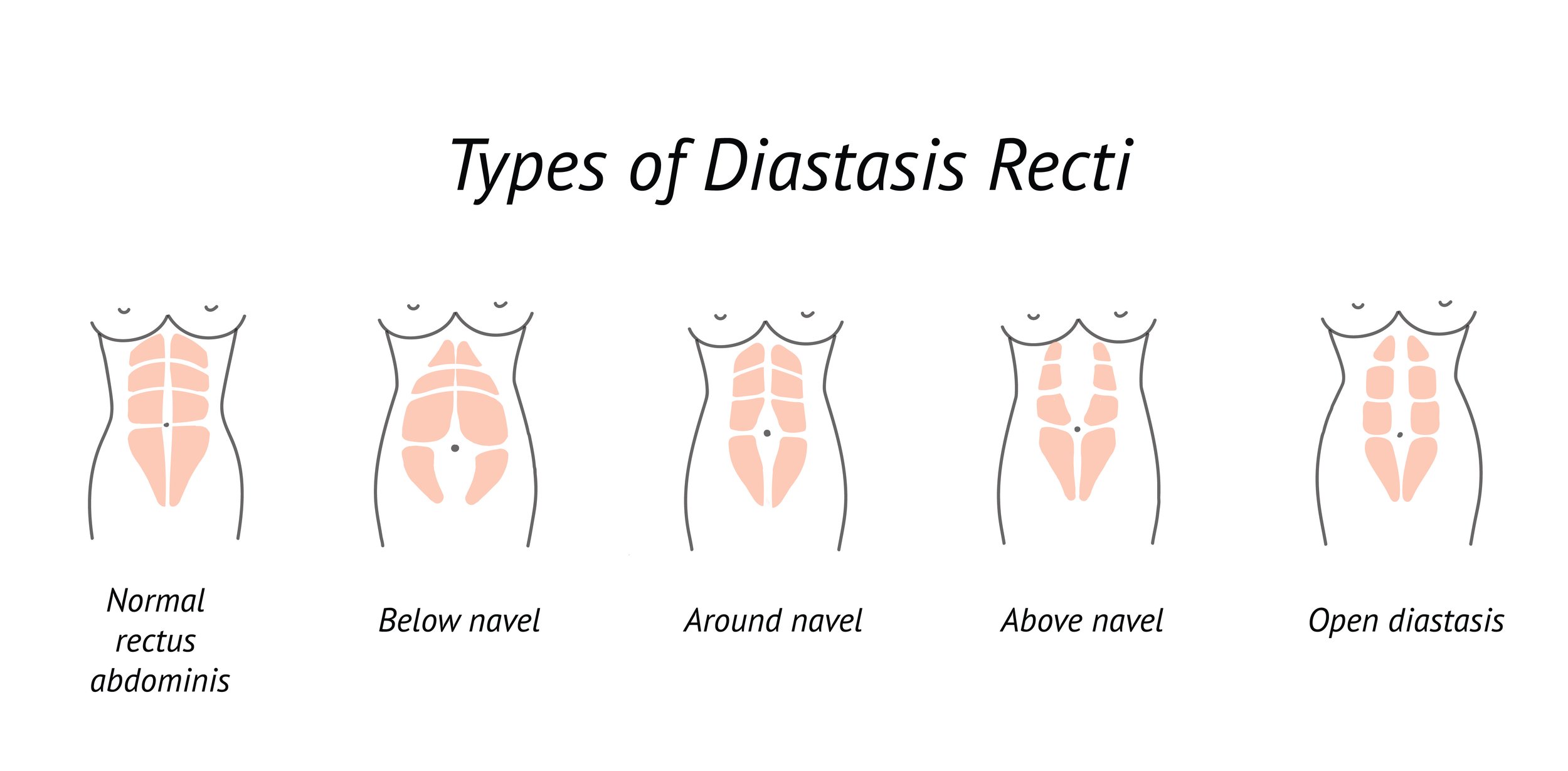
Healing Diastasis Recti: How Hypopressives and Functional Core Training Can Help
To truly restore function to the abdominal wall and core, progressively loading the connective tissue is essential. As Anthony Lo, a leading physiotherapist and expert in strength-based core rehabilitation, states: “Connective tissue needs load to adapt and strengthen. If we avoid loading it, we miss out on its capacity to heal and become more resilient.”
This means that while gentle foundational exercises like breathwork and deep core activation are crucial, progressive resistance and functional movement must also be introduced in a gradual, controlled manner. Increasing load over time through safe and intentional movement encourages the linea alba to regain tension, allowing for improved force transfer, stability, and overall function of the core.
Many traditional abdominal exercises, like crunches and sit-ups, can exacerbate the issue by increasing pressure inside the abdomen, making the gap worse over time. Instead, a functional and pressure-aware approach is needed for true healing.
Understanding and Addressing Queefing: The Role of Alignment and Breathwork
Let’s talk about queefing. Yes, vaginal flatulence—the release of trapped air that can sometimes make an awkward appearance during sex, exercise, or yoga. It’s entirely natural, harmless, but not exactly a confidence booster. Why does it happen, and more importantly, is there something we can do to prevent it? Absolutely. With a deeper understanding of posture, alignment, and breathwork, you can reduce the frequency of queefing and improve overall pelvic health. Let’s dive in.
The Anatomy of the "Just-In-Case" Pee and Why It Matters
Have you ever used the bathroom "just in case" before leaving the house, even if you didn’t really feel the urge to go? Or maybe you’ve squeezed harder when peeing, worrying about leaking or needing to return to the toilet shortly after? These habits might seem harmless, but they can disrupt your bladder’s natural function and contribute to pelvic floor dysfunction over time. Let’s dive into the anatomy behind these common behaviors and how simple techniques like lateral costal breathing, jaw relaxation, and foot positioning can support your bladder’s health.